Hidden Signs of Binge Eating Disorder: Early Treatment Options That Help
This article will help you spot early BED signs and learn about treatment options that can enhance your quality of life. You'll discover various approaches to recovery and healing.

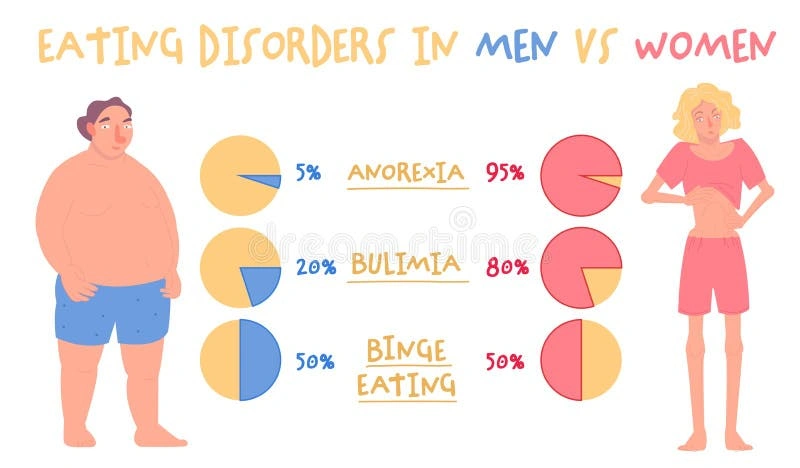
Binge eating disorder (BED) affects roughly 2.8% of U.S. adults at some point in their lives. The disorder stands as America's most common eating disorder, surpassing the combined cases of anorexia nervosa and bulimia nervosa.
BED differs significantly from occasional overeating. People with BED experience chronic, distressing episodes of binge eating at least once weekly for three months or longer. These episodes involve eating large amounts of food faster than normal, usually in secret. Feelings of disgust, guilt, and self-loathing typically follow these episodes. The symptoms of binge eating disorder can be recognized in yourself or someone you care about, and understanding BED's mechanisms helps find the right help.
This piece will help you spot early BED signs and learn about treatment options that can enhance your quality of life. You'll discover various approaches to recovery and healing.
How to Tell the Difference Between Overeating and Binge Eating Disorder
People sometimes eat too much food—maybe during holidays or special celebrations—but knowing when overeating turns into binge eating disorder (BED) needs an understanding of several key differences.
Frequency and intensity of episodes
BED diagnosis requires episodes to occur at least once a week for three months. Regular overeating happens now and then, while BED shows a consistent pattern. The severity of BED depends on how often these episodes happen:
- Mild: 1-3 episodes weekly
- Moderate: 4-7 episodes weekly
- Severe: 8-13 episodes weekly
- Extreme: 14 or more episodes weekly
During these episodes, people eat substantially more food than others would in similar situations, usually within a short two-hour window.
Emotional distress and loss of control
The biggest difference between simple overeating and BED lies in the psychological aspect. People who overeat occasionally can usually control their eating behaviors. On the other hand, BED sufferers feel powerless to stop eating once they start.
This loss of control is central to BED and creates deep distress. People with BED also tend to eat faster, stuff themselves until they're uncomfortable, eat when they're not hungry, and hide their eating habits because they feel ashamed.
Impact on daily life and mental health
Regular overeating barely affects daily functioning, but BED takes a heavy toll on everyday life. The disorder disrupts activities in many areas, with studies showing 46.7% of individuals with BED reporting role impairment and 13.2% reporting severe impairment.
BED often appears alongside other mental health issues. Between 30-80% of people with BED also experience mood or anxiety disorders during their lifetime. These additional conditions make BED treatment more challenging and increase overall distress.
The physical health risks can be serious and include high blood pressure, high cholesterol, type 2 diabetes, and heart disease. Early pattern recognition helps make treatment options for binge eating disorder work better.
Symptoms of Binge Eating Disorder You Shouldn’t Ignore
Identifying warning signs of binge eating disorder is a vital step to get help early. BED is different from just eating too much sometimes - it shows specific patterns that tell us someone needs professional help.
Eating faster and beyond fullness
The most obvious sign of binge eating disorder shows up in how quickly someone eats their food. They might finish meals twice as fast as others and often swallow without chewing properly. People keep eating until they feel uncomfortable or even in pain.
Someone with BED often feels they can't stop eating once they start, whatever physical discomfort they feel. This pattern shows how people lose control - the heart of what makes this disorder so challenging.
Eating when not hungry
The sort of thing I love to point out is how people eat large amounts of food without feeling hungry. Someone might start eating with no appetite or continue long after they're full. We noticed this behavior comes from emotional triggers instead of actual hunger.
Food becomes a way to handle stress, sadness, or anxiety rather than satisfy hunger. This disconnect from natural hunger signals makes it sort of hard to get one's arms around when you're actually hungry versus seeking comfort.
Hiding eating habits from others
BED often makes people very secretive. They might:
- Eat alone because they feel embarrassed
- Hide food in strange places
- Make up stories about missing food
- Plan binges when nobody's around
This hiding comes from deep shame about eating habits and how much food they consume. All the same, trying to keep these secrets usually adds to their emotional burden.
Feeling disgusted or depressed after eating
After binge episodes, people often feel intense self-loathing, guilt, and disgust. They might feel deeply ashamed about how much they ate or feel they lack willpower. These negative feelings create a cycle where depression leads to more binge eating as a way to cope.
The good news is that spotting these signs early helps people get treatment that works for binge eating disorder. Treatment includes therapy that helps with both behavior patterns and the mechanisms behind emotional triggers.
Understanding the Root Causes of BED
Binge eating disorder comes from a mix of biological, psychological, and social factors. We need to understand why it happens to create treatment strategies that work for each person's situation.
Family history and genetics
Your genes play a key role in how likely you are to develop BED. Studies show that people are much more likely to develop an eating disorder when their parents or siblings have had one. This genetic link shows that inherited traits might affect how your brain handles hunger, fullness, and emotions. If your family members have disordered eating patterns, you might face a higher risk of developing BED.
Mental health conditions like anxiety or depression
BED and other mental health issues share a strong connection. Between 30-80% of people with binge eating disorder also experience mood or anxiety disorders during their lifetime. A national study found that 66% of people with BED also struggled with depression. Mental health issues can trigger binge eating, and binge eating can make depression and anxiety worse. This creates a tough cycle that needs professional help to break.
Cultural and body image pressures
Society's expectations about looks and body size often push people toward BED. People who face weight-based discrimination tend to binge eat more often and have higher chances of developing eating disorders. The pressure to meet unrealistic body standards creates mental stress that some people try to handle through disordered eating. This hits harder when you're dealing with different cultural beauty standards at once, as trying to fit multiple ideals can increase stress and make you unhappy with your body.
Stressful life events or trauma
Trauma and major life stress often show up before BED begins. Research shows that about 24% of women with BED also have post-traumatic stress disorder. Stress releases cortisol, which makes you hungrier and crave high-calorie foods loaded with sugar and fat. Many people use binge eating to cope - it helps them numb difficult emotions or avoid painful memories temporarily. But this relief doesn't last, and people often feel more shame and anxiety afterward.
Understanding these basic causes helps find the best treatment for binge eating disorder. Treatment usually needs to tackle both the eating behaviors and what's causing them.
How to Treat Binge Eating Disorder Early
Getting help early is significant to manage binge eating disorder effectively. The right treatment can help break the cycle of binge eating and build healthier relationships with food.
Structured eating routines
Regular meal patterns are the foundations of recovery. Eating consistently every 3-4 hours signals your body about steady nutrition, which prevents powerful cravings that trigger binges. You should eat three meals and three snacks daily to normalize your eating behavior. Planning meals ahead lets you shop mindfully and cuts down anxiety-inducing decisions about food.
Therapy options like CBT and DBT
Cognitive Behavioral Therapy (CBT) remains the most prominent psychological treatment for BED. This method helps break the diet-binge cycle by promoting healthier eating patterns and addressing shape and weight concerns. Dialectical Behavior Therapy (DBT) provides another effective solution that teaches mindfulness, distress tolerance, and emotion regulation skills to handle emotional triggers behind binging.
Medication and psychiatric support
Lisdexamfetamine (Vyvanse) is currently the only FDA-approved medication that treats moderate to severe binge eating disorder in adults. Antidepressants might help some people manage co-occurring conditions like depression or anxiety that often come with BED. Note that medication works best with therapy rather than alone.
Building a support system
People who understand you can substantially reduce binge episodes. Studies show strong support networks minimize stress effects—a common binge trigger. Talk about your challenges with trusted family members or friends, or join support groups where others share similar recovery experiences.
When to seek professional help
Start treatment right away if:
- You use food to cope with stress or loneliness
- Your weight affects your outlook on life
- You're preoccupied with food
- You binge eat or purge
BED can cause serious health complications including cardiovascular issues, acid reflux, and even liver failure if left untreated. Schedule your appointment with Truth and Wellbeing today! Treatment usually needs a team of doctors, therapists, dietitians, and sometimes psychiatrists who work together to tackle all aspects of the disorder.
Conclusion
Binge eating disorder (BED) is a serious condition that affects millions of Americans. Many people don't spot its signs until the disorder has substantially affected their lives. The difference between occasional overeating and BED is a vital first step to recovery. This disorder can lead to severe physical and psychological problems if left untreated and affects almost every part of daily life.
Getting help early makes a big difference in how well treatment works. The warning signs include rapid eating, eating despite feeling full, hiding eating habits, and feeling distressed after binging. People who understand why it happens - whether it's genetics, mental health issues, cultural pressures, or past trauma - can get more tailored treatment that works better.
Getting better takes time and dedication. A combination of regular eating patterns, proven therapies like CBT or DBT, medication if needed, and strong support from others helps break disordered eating patterns. Starting this experience might feel too much at first, but small steps toward better habits create lasting change.
Professional help for binge eating disorder shows strength, not weakness. Many people don't ask for help because they feel ashamed, but proper treatment is a chance to fix your relationship with food. It also helps address the deeper emotional needs that binge eating temporarily fills. You can break free from the cycle of binging and emotional distress that comes with this disorder.
Key Takeaways
Understanding the difference between occasional overeating and binge eating disorder can help you recognize when professional intervention is needed for lasting recovery.
• BED requires episodes at least weekly for 3+ months with loss of control, unlike occasional overeating
• Hidden warning signs include rapid eating beyond fullness, eating when not hungry, and secretive behaviors
• Root causes combine genetics, mental health conditions, cultural pressures, and traumatic experiences
• Early treatment through structured eating, CBT/DBT therapy, and professional support prevents serious complications
• Recovery is possible with proper intervention - don't let shame prevent seeking help from qualified professionals
Binge eating disorder affects 2.8% of adults and is the most common eating disorder in the US. Early recognition and treatment significantly improve outcomes, making it crucial to understand these signs and seek professional help when patterns emerge.
FAQs
Q1. What are the most effective treatments for binge eating disorder? The most effective treatments for binge eating disorder include a combination of structured eating routines, cognitive-behavioral therapy (CBT), and in some cases, medication. Establishing regular meal patterns, learning coping strategies through therapy, and addressing underlying mental health issues are key components of successful treatment.
Q2. How can I distinguish between occasional overeating and binge eating disorder? Binge eating disorder involves frequent episodes (at least once a week for three months) where large amounts of food are consumed rapidly, accompanied by a feeling of loss of control. Unlike occasional overeating, BED significantly impacts daily life and mental health, often involving secrecy and intense feelings of shame or guilt after eating.
Q3. What are some early warning signs of binge eating disorder? Early warning signs include eating rapidly and beyond fullness, consuming food when not physically hungry, hiding eating habits from others, and experiencing intense feelings of disgust or depression after eating. If you notice these patterns occurring regularly, it may be time to seek professional help.
Q4. Can binge eating disorder be treated without medication? Yes, binge eating disorder can often be treated without medication. Many people find success through a combination of psychotherapy (particularly CBT or DBT), structured eating routines, and building a strong support system. However, in some cases, medication may be recommended as part of a comprehensive treatment plan, especially if there are co-occurring mental health conditions.
Q5. How does stress contribute to binge eating disorder? Stress is a significant trigger for binge eating episodes. It can lead to increased cortisol production, which enhances cravings for high-calorie, sugary foods. Many people use binge eating as a coping mechanism for stress or emotional discomfort. Learning healthier stress management techniques is often a crucial part of BED treatment.
%20(1).png)
.png)
%20(1).png)
![The Surprising Science Behind How Anxiety Changes Your Brain [Expert Guide]](https://cdn.prod.website-files.com/67b2977a97f2467db071d9a0/68d19c0eebd18faa7d5c4830_The%20Surprising%20Science%20Behind%20How%20Anxiety%20Changes%20Your%20Brain%20%5BExpert%20Guide%5D%20(1).png)


